CBT for Anxiety: What to Expect During Your Feel Better Therapy Sessions

Learn what Cognitive Behavioural Therapy looks like in practice at Feel Better Therapy and what you can expect from CBT treatment for anxiety.
If you've researched anxiety treatment, you've likely encountered Cognitive Behavioural Therapy. CBT represents the most extensively studied and consistently effective treatment for anxiety disorders, with decades of research supporting its efficacy. But knowing CBT works and understanding what actually happens during sessions are different experiences.
This guide explains what CBT looks like in practice at Feel Better Therapy, how our therapists structure treatment for Irish clients, and what you can realistically expect from the process. Whether you're considering CBT for generalised anxiety, panic disorder, social anxiety, or specific phobias, understanding the framework helps you engage more effectively with treatment.
What CBT Actually Is (And Isn't)
Cognitive Behavioural Therapy operates on a straightforward premise: our thoughts, emotions, and behaviours interconnect, and changing one domain influences the others. Anxious thinking patterns—catastrophising, overestimating threat, underestimating coping capacity—maintain anxiety by shaping both emotional responses and behavioural avoidance.
CBT isn't positive thinking or simply "changing your mindset." It's a structured, skills-based approach that teaches you to identify specific thought patterns contributing to your anxiety, evaluate their accuracy, and develop behavioural responses that reduce rather than reinforce anxious arousal.
The therapy is typically time-limited—most anxiety treatment spans 8 to 16 sessions—though duration depends on symptom severity, comorbid conditions, and individual progress. Unlike open-ended counselling, CBT maintains clear treatment goals and regularly assesses whether those goals are being achieved.
The Structure of CBT Sessions at Feel Better Therapy
While each therapist brings their individual style, CBT follows a consistent structure that maximises therapeutic efficiency. Understanding this structure helps you know what to expect and how to prepare.
Sessions typically begin with a brief mood check and agenda setting. Your therapist asks about your week, any significant anxiety episodes, and what you'd like to focus on. This isn't casual conversation—it identifies material relevant to your treatment goals.
The middle portion addresses specific skills and techniques. Early sessions focus on psychoeducation—understanding how anxiety functions in your body and mind. Middle sessions emphasise skill acquisition—learning cognitive restructuring, exposure techniques, or behavioural experiments. Later sessions concentrate on consolidating gains and preventing relapse.
Each session concludes with summarising key points and assigning between-session work. This homework isn't optional busywork; it's where much of the therapeutic change actually occurs. Practicing skills in your daily life—between sessions, in real anxiety-triggering situations—translates therapy room learning into lived experience.
Cognitive Restructuring: Examining Anxious Thoughts

The "cognitive" component of CBT addresses thinking patterns that maintain anxiety. Your therapist teaches you to identify automatic thoughts—those rapid, often unconscious interpretations that occur in anxiety-provoking situations.
For example, when your manager requests a meeting, you might automatically think "I'm going to be fired." This thought triggers anxiety, which you might manage by avoiding the meeting or over-preparing to compensate. CBT helps you recognise this pattern and evaluate whether the thought reflects reality.
Your therapist guides you through examining evidence for and against anxious thoughts. Has your manager given any indication your performance is unsatisfactory? Have you been fired from previous jobs following routine meetings? What alternative explanations exist—perhaps your manager wants to discuss a new project or provide positive feedback?
This process isn't about forced positive thinking or pretending everything is fine. It's about developing more accurate, balanced thinking that reflects reality rather than anxiety's catastrophic predictions. Sometimes the evidence genuinely supports anxious thoughts—but more often, anxiety exaggerates threat and minimises coping resources.
Behavioural Techniques: Changing What You Do

The "behavioural" component addresses how actions maintain anxiety. Anxious avoidance—steering clear of situations that trigger anxiety—provides short-term relief but long-term maintenance of symptoms. Each avoided situation reinforces the belief that anxiety is intolerable and situations are genuinely threatening.
CBT employs gradual exposure to break this cycle. Your therapist works with you to create an exposure hierarchy—ranking anxiety-provoking situations from least to most challenging. You begin with manageable exposures and progress systematically as your anxiety tolerance builds.
For social anxiety, this might mean initiating brief conversations with strangers, then attending small social gatherings, then speaking in group settings. For panic disorder, exposure might involve deliberately inducing physical sensations similar to panic—rapid breathing, spinning—to learn these sensations aren't dangerous.
The principle is simple but powerful: anxiety diminishes through approaching rather than avoiding feared situations. Each successful exposure provides evidence that you can handle anxiety, that predicted catastrophes don't occur, and that avoidance isn't necessary for safety.
What CBT Looks Like for Different Anxiety Presentations

While CBT's core principles remain consistent, application varies based on your specific anxiety presentation. Your Feel Better Therapy therapist tailors techniques to your particular symptoms and circumstances.
Generalised Anxiety Disorder emphasises worry time scheduling—designating specific periods for anxious rumination rather than allowing it to permeate your entire day—and learning to tolerate uncertainty rather than seeking constant reassurance.
Panic Disorder focuses on interoceptive exposure—deliberately experiencing physical sensations similar to panic attacks—and understanding that panic symptoms, while uncomfortable, aren't medically dangerous.
Social Anxiety targets fear of evaluation through behavioural experiments that test catastrophic predictions about social rejection or judgment, often starting with relatively safe social exposures.
Specific Phobias employ graduated exposure to the feared object or situation, beginning with imaginal or distant exposure and progressing to direct contact as anxiety tolerance develops.
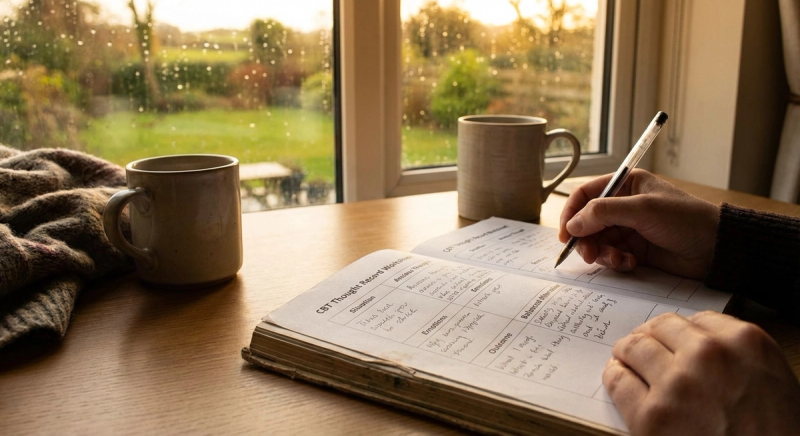
Between-Session Work: Where Change Actually Happens

CBT's effectiveness depends heavily on between-session practice. Your therapist assigns specific exercises—thought records, behavioural experiments, exposure tasks—to complete before your next session. This work translates therapy room learning into real-world application.
Thought records document anxious thoughts as they occur, capturing the triggering situation, automatic thought, emotional response, and alternative balanced thinking. These records reveal patterns invisible during session discussions and provide concrete material for therapy work.
Behavioural experiments test anxious predictions through real-world actions. If you believe "I'll embarrass myself if I speak in the meeting," you might commit to contributing one comment and observing actual outcomes. These experiments generate evidence that often contradicts anxious expectations.
Exposure tasks deliberately approach avoided situations, building anxiety tolerance through repeated, graduated contact. Early exposure feels challenging—this is expected and necessary. With repeated practice, situations that previously triggered intense anxiety become manageable.
Your therapist reviews between-session work at each session, troubleshooting difficulties and celebrating progress. Consistent homework completion strongly predicts treatment success; sporadic practice typically produces disappointing results.
The Timeline: What to Expect Week by Week
CBT for anxiety typically follows a predictable trajectory, though individual variation exists. Understanding this timeline helps set realistic expectations and identify when treatment might need adjustment.
Sessions 1-2 focus on assessment and psychoeducation—understanding your specific anxiety presentation, how CBT addresses it, and establishing treatment goals. You'll likely begin simple monitoring exercises to increase awareness of your anxiety patterns.
Sessions 3-6 emphasise skill acquisition—learning cognitive restructuring, beginning exposure work, and developing anxiety management strategies. This phase often feels most demanding as you're actively challenging established patterns.
Sessions 7-12 concentrate on consolidating skills and addressing remaining symptoms. By this point, many clients experience significant improvement, though individual progress varies. Your therapist assesses whether additional sessions would be beneficial.
Sessions 13+ focus on relapse prevention—maintaining gains after treatment ends, recognising early warning signs of anxiety returning, and having strategies ready for managing future stressors.
CBT's Limitations and When Alternative Approaches Help
CBT effectively treats most anxiety presentations, but it isn't universally appropriate. Some clients find CBT's structured, homework-oriented approach too demanding or insufficiently exploratory. Others have complicating factors—complex trauma histories, personality factors, comorbid depression—that require different or additional approaches.
Feel Better Therapy's matching process considers these factors when pairing you with a therapist. If CBT's structured approach doesn't suit your preferences or needs, we can match you with therapists offering psychodynamic, humanistic, or integrative approaches. Some clients benefit from combining CBT skills with deeper exploratory work.
Your therapist regularly assesses whether CBT is producing expected progress. If significant improvement hasn't occurred within 6-8 sessions, treatment planning is reviewed—perhaps adjusting techniques, addressing complicating factors, or considering alternative approaches.
Preparing for Your First CBT Session
Beginning CBT requires no special preparation, though certain approaches help you engage effectively from the start.
Identify your goals: What would you like to be doing that anxiety currently prevents? Specific, behavioural goals—"attend social gatherings without leaving early," "speak up in work meetings," "reduce daily worry time"—provide clearer treatment targets than vague hopes like "feel less anxious."
Commit to homework: CBT requires between-session practice. Before starting, consider honestly whether you can dedicate time—typically 30-60 minutes daily—to skill practice and exposure tasks.
Embrace temporary discomfort: CBT involves approaching anxiety rather than avoiding it. Early sessions and exposure work often temporarily increase anxiety before producing improvement. This pattern is normal and expected.
Bring specific examples: Rather than general statements like "my anxiety was bad this week," specific situations—"I avoided the team lunch on Tuesday because I feared judgment"—provide concrete material for therapy work.
Related Resources
Understanding CBT represents one aspect of anxiety treatment. You might also be interested in:
- How Feel Better Therapy Matches You with the Right Anxiety Specialist — Understanding our process for pairing you with a therapist whose expertise matches your specific needs
- Affordable Anxiety Support: Understanding Feel Better Therapy's Pricing — Transparent information about session costs and making therapy financially accessible
- Why Feel Better Therapy Chooses Only Fully Accredited Irish Therapists — The accreditation standards ensuring your therapist's qualifications and ethical practice
CBT offers no magic cure for anxiety. What it provides is a structured, evidence-based framework for understanding and addressing the thought patterns and behaviours maintaining your symptoms. With consistent practice and skilled guidance, most people experience significant improvement—often substantial enough that anxiety no longer dominates their daily experience.
The question isn't whether CBT works. The research definitively establishes that it does. The question is whether you're ready to engage with the process—to examine your thinking honestly, to approach rather than avoid anxiety, and to practice skills even when they feel challenging initially.